Diving with Diabetes
By Selene Yeager
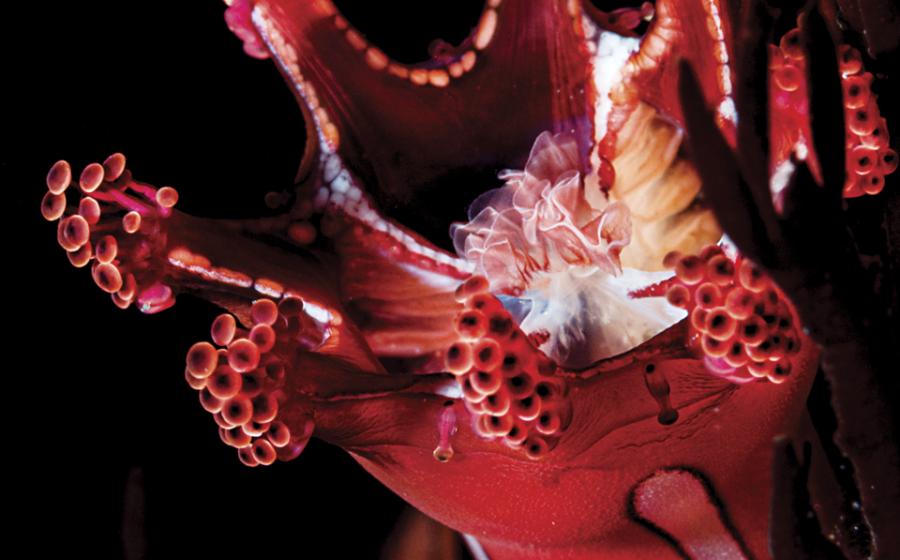
Photo by Joseph Byrd

Diving with diabetes--a condition that can cause dangerously low blood sugar--has been a hotly contested issue nearly as long as there have been recreational divers. In 1975, the UK threw up a red flag, banning men and women with diabetes from diving. Rather than hanging up their BCs, however, many diabetic divers opted to hide their condition and continued secretly diving for decades. Dishonesty is never the best policy (and in diving it can be disastrous), but in this case it paid off. Over the years, word got out that divers with diabetes were racking up thousands of uneventful dives, and in 1991, the British Sub-Aqua Club threw up another red flag for divers with diabetes, only this one had a white diagonal stripe going through it.
Stateside, the YMCA has been certifying otherwise healthy divers with well-controlled diabetes for more than 10 years. But many dive operators continue to put diabetes on their blacklist, forcing those with the disease either to stay ashore or keep it under cover. The Divers Alert Network would like that to change. In a joint workshop with the Undersea and Hyperbaric Medical Society in 2005, DAN and UHMS reached a consensus that people with diabetes, who are otherwise fit, healthy and meet certain safety criteria, can step out into the open and take the plunge.
"We've done studies and found no adverse events. There are people with diabetes running marathons and piloting planes. It's time that we decriminalize diabetes in diving and open the door for a growing population of divers to participate in the sport honestly and safely," says consensus co-organizer Neal Pollock, Ph.D., of the Center for Hyperbaric Medicine and Environmental Physiology, Duke University Medical Center. Pollock co-authored Diabetes and Recreational Diving: Guidelines for the Future.
A Qualified OK
Before you dust off your C-card, know that an open-door policy doesn't mean everyone can just walk right in. Pollock stresses that while diabetes alone doesn't prevent you from diving, other related conditions may. "You have to be in good physical shape and on top of your condition," he says. You also can't have diabetes-related conditions like vascular disease.
DAN has established a list of guidelines you can check out on its web site. Just go to diversalertnetwork.org and type diabetes in the search engine, and you'll find a downloadable pdf. The bottom line is people with diabetes need to be fit to dive, need to choose their dives carefully, and need to manage their diabetes on the day of the dive.
Here's a snapshot of the new rules:
»Dive fitness. "The criteria for diver fitness for people with diabetes isn't all that different from that for typical healthy divers," says Pollock. "The underwater environment doesn't have any special effects on glucose utilization and blood sugar levels. If your diabetes is well-managed during everyday activities on dry land, you're generally safe to dive."
Above all, that means you must be stable with your insulin regimen. You should wait three months after starting oral hypoglycemic agents (OHAs) and one year after starting insulin therapy before your first dive. You should also be free of any serious episodes (meaning you needed outside assistance) of hypoglycemia or hyperglycemia for one year before diving.
If you're prone to seizures, lack of coordination or impaired judgment when your blood sugar drops, you shouldn't dive. Nor should you dive if you don't know how exercise affects your blood sugar or if you can't sense when an episode of low blood sugar is coming on. Losing your faculties 40 feet below can have dire consequences.
Finally, certain diabetes-related health conditions can increase your risk for decompression sickness or other life-threatening complications. Don't dive if you have asthma, neuropathy (nerve damage), nephropathy (kidney disease), retinopathy (eye disease) or heart disease.
»Dive selection. "We still don't have all the information we would like on diving with diabetes under every circumstance," says Pollock. "For that reason, we want to be sure we avoid augmenting the risk by allowing divers to enter precarious situations."
It's a good idea to avoid cold, long, arduous dives that could send your blood sugar spiraling. Shallow diving is your best bet. Avoid anything deeper than 100 feet. "Once you get into the territory where nitrogen narcosis is a risk, it could be confused with hypoglycemia," says Pollock. You also want to avoid decompression dives, because if you have to come to the surface to address a bout of hypoglycemia, you don't want to have to prolong treatment for a decompression stop. Keep your dives to 60 minutes or less in duration, so you're not going unmonitored for an extended period of time. And stay away from wrecks and other overhead environments. The easier it is for you to surface relatively quickly if you need to, the better.
»Dive day management. You need to check your blood sugar before and after every dive to be sure it's in a safe range and not heading south. DAN recommends checking it 60 minutes, 30 minutes and 10 minutes before making a dive, and then once immediately after you get back in the boat or on shore. Your blood sugar should be at least 150 mg.dL (8.3 mmol.L). If it's less than that or if your blood sugar level falls between two of the measurements, you're not safe to take the plunge at that time. Also stay ashore if your blood sugar is too high (above 300 mg.dL or 16.7 mmol.L). Continue to check your blood sugar frequently 12 to 15 hours after diving.
Multiple dives aren't a problem, so long as you follow this same protocol for each dive and you stay stable and don't notice any downward trends. Researchers have had divers make up to four dives a day and found that in people with well-managed diabetes, blood glucose barely budged. That said, there's some evidence that people with diabetes are at increased risk for decompression sickness, so dive conservatively and limit your dives to shorter times than the maximum allowances on the dive tables or dive computer.
Staying Safe
Always carry rescue meds when you dive. Some diabetic divers swear by Insta-Glucose because its sturdy packaging stands up to salt water and changes in pressure. But cake frosting or other sources of oral glucose work, too. Just in case yours accidentally gets swept away by the sea, be sure your buddy carries a spare sugar source for you. DAN also strongly recommends divers with diabetes have parenteral glucagon available at the surface.
Be sure to educate your buddy. The sign for low blood sugar is an "L" with your thumb and index finger. If you feel a hypoglycemic episode coming on underwater, signal your buddy (and the dive leader, who can decide how to handle the rest of the group), and both you and your buddy should swim to the surface. Inflate your BC, take your glucose, and get out of the water. It's best if your buddy does not also have diabetes. Though the odds of both of you having an episode are low, it's wise not to take unnecessary risks.
Finally, take care of yourself. Staying out all night eating nachos and doing flaming shooters at the beachside bar is clearly a bad way to manage blood sugar. Sleep well, eat well, stay hydrated, and absolutely, positively avoid hangovers. That's good advice for anyone.
By Selene Yeager
Photo by Joseph Byrd

Diving with diabetes--a condition that can cause dangerously low blood sugar--has been a hotly contested issue nearly as long as there have been recreational divers. In 1975, the UK threw up a red flag, banning men and women with diabetes from diving. Rather than hanging up their BCs, however, many diabetic divers opted to hide their condition and continued secretly diving for decades. Dishonesty is never the best policy (and in diving it can be disastrous), but in this case it paid off. Over the years, word got out that divers with diabetes were racking up thousands of uneventful dives, and in 1991, the British Sub-Aqua Club threw up another red flag for divers with diabetes, only this one had a white diagonal stripe going through it.
Stateside, the YMCA has been certifying otherwise healthy divers with well-controlled diabetes for more than 10 years. But many dive operators continue to put diabetes on their blacklist, forcing those with the disease either to stay ashore or keep it under cover. The Divers Alert Network would like that to change. In a joint workshop with the Undersea and Hyperbaric Medical Society in 2005, DAN and UHMS reached a consensus that people with diabetes, who are otherwise fit, healthy and meet certain safety criteria, can step out into the open and take the plunge.
"We've done studies and found no adverse events. There are people with diabetes running marathons and piloting planes. It's time that we decriminalize diabetes in diving and open the door for a growing population of divers to participate in the sport honestly and safely," says consensus co-organizer Neal Pollock, Ph.D., of the Center for Hyperbaric Medicine and Environmental Physiology, Duke University Medical Center. Pollock co-authored Diabetes and Recreational Diving: Guidelines for the Future.
A Qualified OK
Before you dust off your C-card, know that an open-door policy doesn't mean everyone can just walk right in. Pollock stresses that while diabetes alone doesn't prevent you from diving, other related conditions may. "You have to be in good physical shape and on top of your condition," he says. You also can't have diabetes-related conditions like vascular disease.
DAN has established a list of guidelines you can check out on its web site. Just go to diversalertnetwork.org and type diabetes in the search engine, and you'll find a downloadable pdf. The bottom line is people with diabetes need to be fit to dive, need to choose their dives carefully, and need to manage their diabetes on the day of the dive.
Here's a snapshot of the new rules:
»Dive fitness. "The criteria for diver fitness for people with diabetes isn't all that different from that for typical healthy divers," says Pollock. "The underwater environment doesn't have any special effects on glucose utilization and blood sugar levels. If your diabetes is well-managed during everyday activities on dry land, you're generally safe to dive."
Above all, that means you must be stable with your insulin regimen. You should wait three months after starting oral hypoglycemic agents (OHAs) and one year after starting insulin therapy before your first dive. You should also be free of any serious episodes (meaning you needed outside assistance) of hypoglycemia or hyperglycemia for one year before diving.
If you're prone to seizures, lack of coordination or impaired judgment when your blood sugar drops, you shouldn't dive. Nor should you dive if you don't know how exercise affects your blood sugar or if you can't sense when an episode of low blood sugar is coming on. Losing your faculties 40 feet below can have dire consequences.
Finally, certain diabetes-related health conditions can increase your risk for decompression sickness or other life-threatening complications. Don't dive if you have asthma, neuropathy (nerve damage), nephropathy (kidney disease), retinopathy (eye disease) or heart disease.
»Dive selection. "We still don't have all the information we would like on diving with diabetes under every circumstance," says Pollock. "For that reason, we want to be sure we avoid augmenting the risk by allowing divers to enter precarious situations."
It's a good idea to avoid cold, long, arduous dives that could send your blood sugar spiraling. Shallow diving is your best bet. Avoid anything deeper than 100 feet. "Once you get into the territory where nitrogen narcosis is a risk, it could be confused with hypoglycemia," says Pollock. You also want to avoid decompression dives, because if you have to come to the surface to address a bout of hypoglycemia, you don't want to have to prolong treatment for a decompression stop. Keep your dives to 60 minutes or less in duration, so you're not going unmonitored for an extended period of time. And stay away from wrecks and other overhead environments. The easier it is for you to surface relatively quickly if you need to, the better.
»Dive day management. You need to check your blood sugar before and after every dive to be sure it's in a safe range and not heading south. DAN recommends checking it 60 minutes, 30 minutes and 10 minutes before making a dive, and then once immediately after you get back in the boat or on shore. Your blood sugar should be at least 150 mg.dL (8.3 mmol.L). If it's less than that or if your blood sugar level falls between two of the measurements, you're not safe to take the plunge at that time. Also stay ashore if your blood sugar is too high (above 300 mg.dL or 16.7 mmol.L). Continue to check your blood sugar frequently 12 to 15 hours after diving.
Multiple dives aren't a problem, so long as you follow this same protocol for each dive and you stay stable and don't notice any downward trends. Researchers have had divers make up to four dives a day and found that in people with well-managed diabetes, blood glucose barely budged. That said, there's some evidence that people with diabetes are at increased risk for decompression sickness, so dive conservatively and limit your dives to shorter times than the maximum allowances on the dive tables or dive computer.
Staying Safe
Always carry rescue meds when you dive. Some diabetic divers swear by Insta-Glucose because its sturdy packaging stands up to salt water and changes in pressure. But cake frosting or other sources of oral glucose work, too. Just in case yours accidentally gets swept away by the sea, be sure your buddy carries a spare sugar source for you. DAN also strongly recommends divers with diabetes have parenteral glucagon available at the surface.
Be sure to educate your buddy. The sign for low blood sugar is an "L" with your thumb and index finger. If you feel a hypoglycemic episode coming on underwater, signal your buddy (and the dive leader, who can decide how to handle the rest of the group), and both you and your buddy should swim to the surface. Inflate your BC, take your glucose, and get out of the water. It's best if your buddy does not also have diabetes. Though the odds of both of you having an episode are low, it's wise not to take unnecessary risks.
Finally, take care of yourself. Staying out all night eating nachos and doing flaming shooters at the beachside bar is clearly a bad way to manage blood sugar. Sleep well, eat well, stay hydrated, and absolutely, positively avoid hangovers. That's good advice for anyone.