An Undiagnosed Heart Issue | Lessons for Life
Carol sensed something was wrong as she reached the boat. She wasn’t sure what was going on, but she knew she had to get back on board. As she pulled herself up the ladder her right arm jerked. Everything went dark.

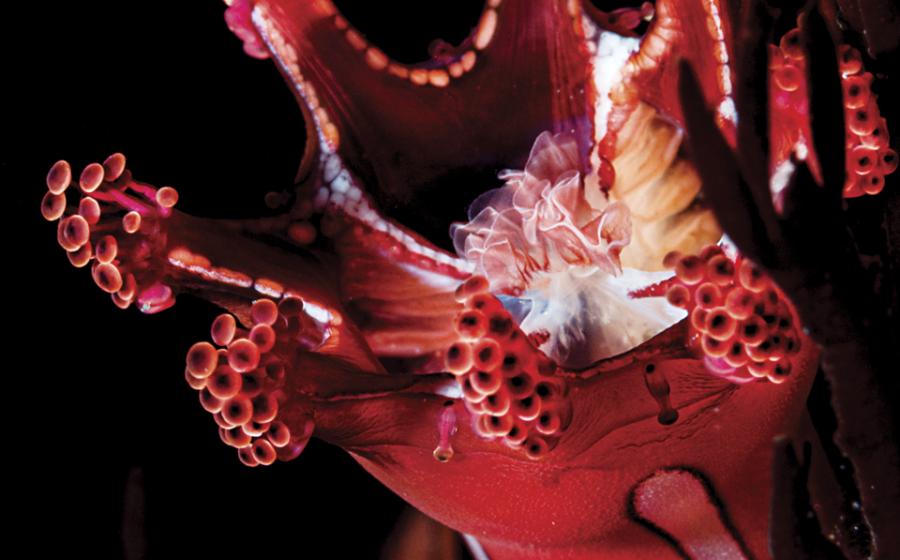
Carlo GiambarresiPFOs can present a problem in scuba divers.
THE DIVES
The trip started out great. Carol—a 50-year-old with 87 lifetime dives and good overall health—planned two days of diving and was having fun. On day one, she completed two dives with a max depth of 130 feet. She started deep on both dives and worked her way into shallower waters on the coral reef for about 30 minutes each. That night she felt fine, although she did have a mild headache. She attributed it to trouble with her sinuses and clearing her ears. She took some sinus medication with a pain reliever and went to bed. Carol’s dives for the second day were shallower, with a max depth of 45 feet on both dives for about 30 minutes each. Her surface interval between the two dives lasted about 45 minutes.
THE ACCIDENT
On the surface, Carol noticed spasms in her right arm, and she felt lightheaded as she climbed out of the water. At the top of the steps everything went dark. Carol lost consciousness and fell backward into the water in full gear. Fortunately, there was no one too close behind her in the water.
The boat crew jumped in and grabbed Carol before she could float away. They pulled her out of her gear and lifted her into the boat. She was still breathing and slowly regained consciousness after the crew placed her on 100 percent oxygen.
The boat captain notified the U.S. Coast Guard. Once the other divers were on board, the captain arranged to meet up with a Coast Guard fast boat, which took Carol directly to a waiting ambulance on the shore.
Upon examination at the hospital, Carol was alert and oriented. That means she could identify who she was, where she was, what day it was and what happened to her.
In medical parlance, that is alert and oriented times four. When a person can’t answer those questions, there is a concern with mental status; this is the first series of questions asked in a field neurological exam.
On further examination, the doctor discovered that Carol’s involuntary right arm spasms were still present. She was also unsteady on her feet. The doctor determined Carol had short-term memory loss and slurred speech. She was also hyperglycemic.
The doctor ordered Carol to be transferred to a local hyperbaric chamber, where she was treated with three U.S. Navy Treatment Table 6s over consecutive days. All of her neurological symptoms—the unsteady gait, memory loss and speech problems—disappeared after the third treatment. It took several months for the muscle spasms in her right arm to clear up.
ANALYSIS
Carol discovered two medical issues during the process. She had Type 2 diabetes, which accounted for the hyper-glycemia. She began a regimen of diet, exercise and medical treatment that brought her blood sugar under control. The hyperglycemia likely was unrelated to Carol’s diving incident, although it might have been related to the headaches and possible dehydration from excessive urination.
In general, divers with well-controlled diabetes can continue to dive, but they have to take special precautions, including carrying oral glucose paste on dives. For more specifics and recommendations, contact a doctor familiar with diving.
Most importantly for this situation, however, Carol had an undiagnosed patent foramen ovale in her heart.
In utero, oxygenated blood comes from the placenta and not from the lungs. So our hearts have an opening that allows blood to flow between the two top chambers (the atria), thus bypassing the lungs. This opening, which is actually a flap, is a called the foramen ovale. At birth, when the lungs expand, this flap closes permanently and venous blood is then routed to the lungs to receive oxygen in about 75 percent of people. However, in approximately 25 percent of people this flap remains open and can allow venous blood from the right side of the heart to cross over to the left side of the heart.
PFOs can present a problem in scuba divers. When a diver performs a Valsalva maneuver, there is an increase in pressure in the right side of the heart. This also happens during an exertion like climbing up a ladder to get out of the water or straining to lift a weight. That increase in right heart pressure can cause the PFO to open and allow blood from the venous side of the heart to pass over into the arterial side.
This still isn’t normally a big problem, unless the diver also has a significant nitrogen gas load. In that case, the transfer of blood allows nitrogen gas bubbles to pass from the venous side, which would have been filtered out in the lungs, over into the arterial side. The nitrogen bubbles are then distributed to the body. That can cause those bubbles to lodge in joints, in the nervous system or in the brain, causing strokelike neurological symptoms— just like Carol exhibited.
In Carol’s case, the dives from her first day exceeded the U.S. Navy Dive Table limits for no-deco diving based on a square profile. Her dives on the second day were well within diving limits but may have compounded the problem by not allowing her body to completely off-gas the high nitrogen load. The combination of the increased nitrogen gas load, PFO, exertion of climbing out of the boat, dehydration and hyperglycemia created the perfect set of circumstances.
Options for divers with recurrent decompression sickness and a diagnosed PFO include: stopping scuba diving, diving conservatively or having the PFO closed.
Closing a PFO is an outpatient non-surgical procedure that can be performed in about an hour. Patients usually go home the same day and are usually treated with a combination of aspirin and a blood thinner for a period of three to six months. It is recommended that the patient then under- goes a repeat echocardiogram with injection of agitated saline (bubble study). If no shunt is present, the patient may be able to return to diving without restrictions.
In this situation, Carol tested positive for a PFO and went through a procedure to close it. Just under two years after her incident she returned to diving. At a follow-up, she had completed 30 more dives without any problem.
Many thanks to interventional cardiologist, technical diver and dive instructor Dr. Douglas Ebersole at the Watson Clinic in Lakeland, Florida, for his input on this column.
LESSONS FOR LIFE
• Pay close attention to your health and discuss potential problems with your doctor.
• Don’t push the dive tables. Diving a table to the limits, even on multilevel dives or using a computer, raises your risk of decompression illness.
• Give the diver ahead of you room to climb up the ladder.
• Understand the signs and symptoms of decompression illness and how to identify them. Take training in field neurological assessment and oxygen first aid.
• If you have multiple, unexplained cases of decompression illness, talk to a doctor familiar with diving medicine about the possibility of a PFO.