A Curious Case | Lessons for Life
About 60 minutes after he surfaced from his second dive, Ted knew something was wrong. He was sick to his stomach, and he couldn’t stand up. He didn’t know what was going on, but nothing about his symptoms made sense.
Steven P. HughesTed, the diver involved was a 54-year-old active diver with no known medical conditions.
THE DIVER
Ted was a 54-year-old active diver with no known medical conditions. He had been diving for nearly 20 years and regularly took trips to remote locations where he dived heavily for days in a row.
THE DIVES
Ted and his buddy had planned a series of dives over three days with a charter company. They regularly visited the destination and were familiar with the dive sites and the crew of the operation. Ted’s dives included the following:
• Day 1: Dive #1, 67 feet of seawater (fsw) for 42 min with a surface interval of 58 min; Dive #2, 58 fsw for 46 min.
• Day 2: Dive #1, 137 fsw for 29 min with a surface interval of 80 min; Dive #2, 82 fsw for 41 min with a surface interval of 73 min; Dive #3, 54 fsw for 50 min.
• Day 3: Dive #1, 132 fsw for 25 min with a surface interval of 122 min; Dive #2, 109 fsw for 36 min.
We don’t know their gas mixes nor their decompression schedules.
THE ACCIDENT
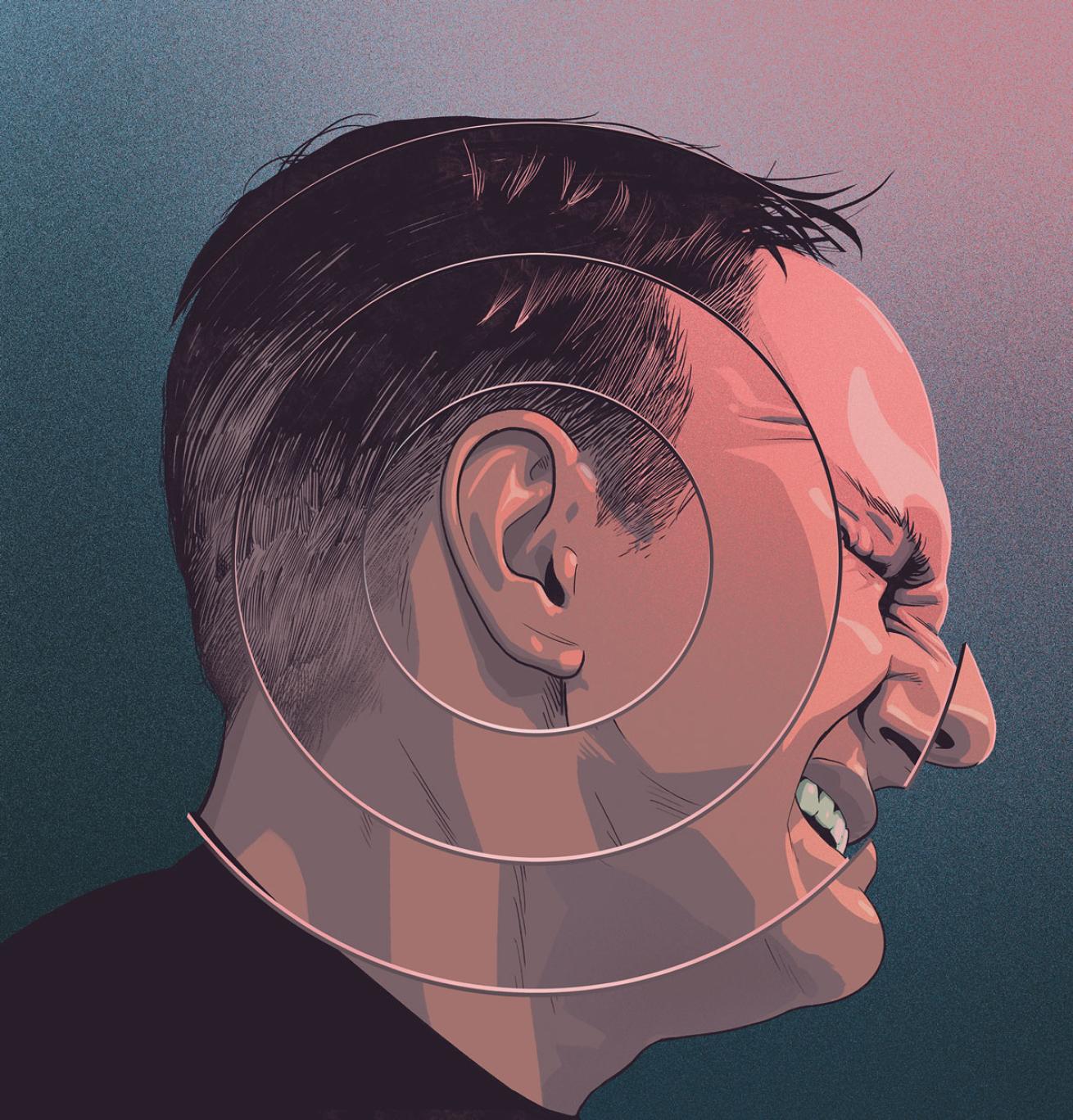
Ted and his buddy had planned a third dive for their last day, but Ted didn’t feel well and opted out. After an hour at the surface, he felt dizzy and nauseous. Even simple head movements made him so sick he would vomit. It felt like a sudden onset of seasickness, but if he remained still his stomach settled down.
He couldn’t walk without support. Concerned about the possibility of decompression sickness, the crew administered 100 percent oxygen first aid, but Ted’s symptoms didn’t change. The crew immediately notified EMS and began heading for the dock. Ted was transported to the emergency department of a local hospital.
The attending physician gave Ted a thorough physical exam, including a detailed neurological assessment, and examined Ted’s ears for signs of barotrauma. All the exams came back negative. Even under continued oxygen first aid, Ted’s symptoms did not improve. He had to stay completely still in a partially reclined position or he would vomit. Given the persistent symptoms and the lack of barotrauma, the doctor determined Ted was suffering from inner ear decompression sickness.
The hospital had a hyperbaric chamber and immediately began treating Ted with a U.S. Navy Treatment Table 6. Following the first treatment, Ted was able to stand without help. He was still nauseous, but it didn’t cause him to vomit. He was not able to walk heel-to-toe, however. Ted received a second Table 6 the next morning and saw further relief. He was still unsteady but was able to walk heel-to-toe. His nausea was gone. The next day, Ted received a U.S. Navy Treatment Table 5. Afterward, he was completely free of symptoms. He was released from the hospital and flew home three days later with no problems.
ANALYSIS
Every diver learns a little bit about the possibility of decompression sickness (DCS) in their open-water diver training, but for most it is something they never face. Even today, more than 110 years since John Scott Haldane created the first diving decompression tables, a lot is still unknown about the condition.
Generally, researchers believe DCS is caused by accumulation of nitrogen in the body tissues and bloodstream. As divers ascend and lower the ambient pressure on their bodies, nitrogen comes out of the tissues and can form bubbles.
Those nitrogen bubbles can block blood flow, causing pain in the joints or putting pressure on nerves, causing severe symptoms including paralysis and death.
Inner ear decompression sickness (IEDCS) is a relatively rare manifestation of DCS. It is thought that bubbles actually form in the cochlea and semicircular canals of the inner ear. These structures are instrumental to hearing and balance. The formation of bubbles in the fluid in the inner ear can cause extreme vertigo, nausea and the inability to walk. The inability to walk heel-to-toe, also referred to as tandem gait, is an indication of several things including alcohol intoxication and vertigo.
Even though nitrogen bubbles can form in numerous locations in the body with varying effects, the clinical treatment for DCS is fairly standard. The U.S. Navy developed a series of treatment protocols called treatment tables; U.S. Navy Treatment Table 6 is by far the most commonly used for DCS. In its basic form, it is four hours and 45 minutes long, although that can be extended. The diver spends time at 60 feet and then 30 feet, breathing 100 percent oxygen. U.S. Navy Treatment Table 5 is a shorter oxygen table, typically used for pain-only decompression sickness and as a final treatment to make sure a diver’s symptoms are gone.
In the field, in cases of DCS the standard of care for an injured diver is breathing the highest concentration of oxygen possible. The gold standard is 100 percent oxygen through a mask and a demand valve, similar to a scuba regulator. The inhaled oxygen creates a greater imbalance in the body, helping to remove nitrogen from the blood and body tissues faster. Any inspired nitrogen will slow that gas movement.
A positive response to oxygen first aid is also a solid indicator of DCS. Often, divers exhibit symptoms only to have them go away while breathing oxygen. The return of those symptoms when the oxygen first aid is discontinued is a positive sign that a diver’s symptoms are related to diving.
In Ted’s case, breathing oxygen didn’t relieve his symptoms. Inner ear DCS is extremely difficult to treat because of the low amount of gas exchange in inner ear fluids compared to the bloodstream. The combination of symptoms, along with the diving profiles Ted had completed, is what led the treating doctor to believe Ted had IEDCS.
Without knowing Ted’s breathing gases and his decompression schedules, it is impossible to judge if Ted was over the limits when it came to his diving. Still, these are aggressive dive profiles, especially on the second and third days. A recreational diver using air would definitely be at an elevated risk; a technical diver with gas mixtures appropriate to these depths and with planned decompression could be well within risk limits.
Any unusual symptoms following a dive—even if not as dramatic as Ted’s— should give you cause for concern. Alert the boat crew, and watch for other symptoms that may indicate a larger problem.
LESSONS FOR LIFE
■ Dive within the limits of your training. If you are interested in diving deeper or longer, or using specialty gas mixes, seek out the appropriate training.
■ Understand the signs and symptoms of decompression sickness. This is true for yourself and in other divers. Divers will often try to ignore symptoms, writing them off as something else, making the condition more difficult to treat.
■ Oxygen first aid. Learn to administer oxygen first aid, and have the equipment available when you need it.
Douglas Ebersole — an interventional cardiologist at the Watson Clinic in Lakeland, Florida, director of the Structural Heart Program at Lakeland Regional Health Medical Center and a cardiology consultant to Divers Alert Network—assisted with this column.
Read more Lessons for Life here.
More from the Author
Poached: Fighting for Sea Turtles | A Mike Scott short story by Eric Douglas
When photojournalist Mike Scott stumbles across a man stealing sea turtle eggs, he jumps into action, unraveling a network of wildlife smugglers. The latest in Eric Douglas’ Mike Scott dive adventure thrillers, this four-part series rolled out in June 2020. Each installment includes tips to help you protect sea turtles too.